Paula and Bobby
Parents of Lillie
Pierpont syndrome
What is Pierpont syndrome?
It is a rare genetic syndrome that affects multiple parts of the body. Most of the features associated with the syndrome are congenital, meaning they are present at birth. Unique facial features and limb anomalies are characteristics of the syndrome.
This syndrome is also known as:
Pierpont (1998) - plantar lipomatosis-unusual face Pierpont Syndrome
What gene changes cause Pierpont syndrome?
Changes to the TBL1XR1 gene are responsible for causing the syndrome.
The syndrome is inherited in an autosomal dominant pattern.
What are the main symptoms of Pierpont syndrome?
The main facial features of the syndrome include a very small head, a small jaw, widely spaced eyes, a prominent forehead, deeply set eyes, crossed eyes, a broad nasal tip, short nose, full cheeks, large and fleshy ears and a short neck.
Physical features of the syndrome include short digits (fingers and toes), short and broad palms and a short stature.
Intellectual disability and developmental delay are also symptoms of the syndrome. Specifically speech and language delay which is common with the syndrome.
Other symptoms of the syndrome include reduced muscle tone, seizures, scoliosis (abnormal curving of the spine), feeding issues, a failure to thrive and a reduced weight.
How does someone get tested for Pierpont syndrome?
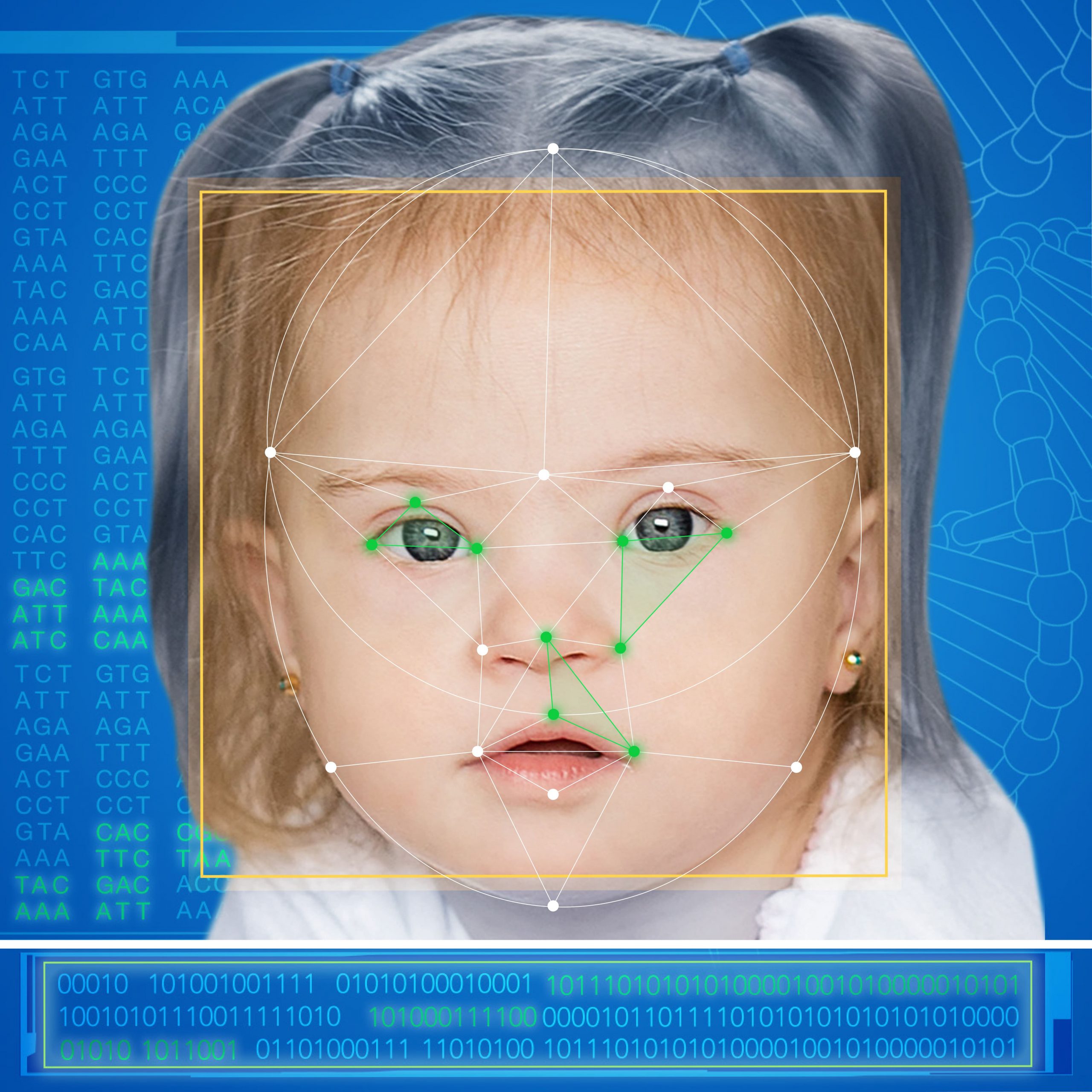
The initial testing for Pierpont syndrome can begin with facial analysis screening with FDNA’s AI technology, which can identify the key markers of the syndrome and outline the need for further testing.
Based on clinical consultation with a genetic professional, different options for genetic testing will be proposed.
Información médica sobre Pierpont syndrome
Pierpont syndrome is characterized by the combination of dysmorphic features (high forehead, underdeveloped mid-face, narrow palpebral fissures and anteverted nares), short stature, hearing loss, developmental delay and distinctive palmar and plantar fat pads.
Pierpont et al. (1998) reported two unrelated children. They both had unusual congenital fat pads on the anteromedial aspect of the heels together with prominent fetal pads on the fingertips and deep palmar and plantar grooves with pillowing of the areas between the grooves. The facies were distinctive with a prominent forehead, mild microcephaly, mid-face hypoplasia, a squared off nasal tip, a thin upper lip, anteverted nostrils, and a central palatal ridge. Both children were developmentally delayed. Further features were widely spaced teeth. One child had grand mal and myoclonic seizures starting at the age of five years. The chromosomes were reported as normal in one child, but skin chromosomal analysis was not mentioned in the other child.
A second report of this condition has been published by Oudesluijs et al., 2005. There were feeding problems and moderate developmental delay. At seven months the skin over the hands and feet was excessive and palmar and plantar grooves were deep with pillowing. The fatty pads were located on the medial border of the feet. Facially, the forehead was high, with remarkably narrow and upslanting palpebral fissures, there was a broad nasal bridge and tip, a bowed upper lip, full cheeks and a prominent lower lip. There was mild midfacial hypoplasia.
Seven additional patients were reported by Burkitt Wright et al., (2011). There was also some follow up of previously reported patients. It is of interest to note that in some, the fat pads disappeared later in childhood.
Heinen et al. (2016) reported six unrelated individuals with Pierpont syndrome, ranging in age from 5.7 to 28 years. The disorder was caused by a single heterozygous missense variant, c.1337A>C (p.Tyr446Cys), in TBL1XR1. Growth was decreased. Dysmorphic features included high forehead, narrow palpebral fissures, flat malae, broad nasal ridge and tip, thin upper vermillion and large ears, marked grooves and pillowing of hands and feet, subcalcaneal fat pads and scoliosis. Hearing loss was detected in five out of six patients. Intellectual disability was moderate to severe (IQ up to 60). Brain imaging showed enlarged ventricles in two patients and choroid plexus papilloma in one patient.
Kahlert et al. (2017) described a patient with Pierpont syndrome due to the same recurrent c.1337A > G (p.Tyr446Cys) mutation in the TBL1XR1 gene. Additional to common Pierpont syndrome clinical characteristics the patient had microphthalmia, pendular nystagmus, cryptorchidism, dermal sinus, and peripheral joint laxity.
Slavotinek et al. (2017) described a seven years old male with Pierpont syndrome. He was born after the pregnancy, complicated by hypertension and hyperemesis. The patient had profound intellectual disability, hypotonia, frequent ear infections and chronic constipation. Facial dysmorphism included high anterior hairline, small eyes with narrowed palpebral fissures, a bulbous nasal tip with a short columella, large mouth with a thin upper vermilion, and small chin. He also had a submucous cleft palate, bilateral cryptorchidism, hydronephrosis, multiple bilateral renal cysts and calyceal diverticula. He had small nails; his palms and soles had deep creases and pillowing of the soft tissues. Skeletal findings included prominent left side of the chest, thoracolumbar scoliosis, slightly flexed elbows, bilateral talipes, camptodactyly of the second to fifth fingers and short second and fifth toes with second toes overlapping third toes bilaterally. Brain MRI showed Arnold Chiari malformation that was also present in his maternal uncle. The authors identified the same de novo TBL1XR1 gene mutation that was previously reported in other Pierpont syndrome cases.
* This information is courtesy of the L M D.
If you find a mistake or would like to contribute additional information, please email us at: [email protected]
FDNA™ Health can help you with the diagnostic journey.
Aprenda sobre los retrasos en el desarrollo infantil: Causas, Síntomasy Terapias.
No espere años para un diagnóstico. Actúe ahora y ahorre un tiempo valioso.
Qué es FDNA Health?
With the largest global database and a leading decision-support tool using AI, FDNA™ Health enables patients and their families to better understand symptoms and conditions with the goal of shortening the time to diagnosis.
Beneficios de FDNA Health
Ahorre un tiempo valioso al
aprender acerca de las posibles condiciones
e informe a su médico
Tecnología avanzada de IA
y médicos líderes en todo el mundo
acortar el tiempo hasta el diagnóstico
¿Buscas respuestas?
¿Preocupado por el desarrollo infantil?
¡Estamos aquí para ayudarte!